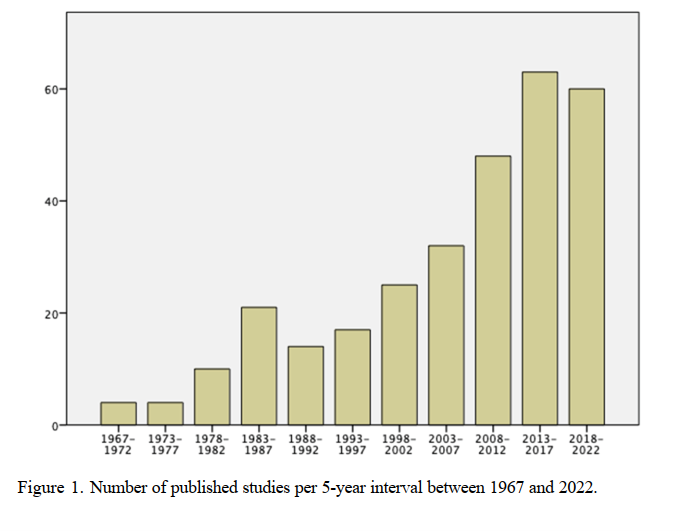
Let us return to quantitative studies of PDT. The first one emerged in 1967 (Gelder et al., 1967). Between 1970 and 2020, each decade yielded 15, 30, 40, 60 and 120 RCT:s, an accelerating development. Between 2020 and 2023 55 studies were published. A Swedish researcher, Peter Lillliengren, is continually listing quantitative PDT studies. You’ll find the latest version here. The diagram below shows, per five-year-period, the almost 300 Randomized Controlled Trials so far published.
Several meta-analyses of these studies (Abbass et al., 2013; Anderson and Lambert, 1995; Barth et al., 2013; Cristea et al., 2017; Cuijpers, 2017; Cuijpers et al., 2008, 2013, 2016; Driessen et al., 2020, 2022, 2015; Leichsenring and Rabung, 2008, 2011; Keefe et al., 2014, Kivlighan III et al., 2015; Leichsenring et al., 2022, Steinert et al., 2017) have shown largely similar results across different forms of therapy. Lilliengren (2023) summarizes: “PDT typically outperforms inactive controls, while comparisons with active treatments, including Cognitive-Behavior Therapy (CBT), typically indicate no statistical difference… There is a pressing need for disseminating the existing research for PDTs to policy makers and the general public, as well as integrating findings in psychodynamic training curriculums”.
In recent years, PDT has struggled to be heard in the PR battle against other forms of therapy. It’s a shame because Lilliengren’s article and the cited meta-analyses show that research support is generally good for both PDT and CBT. However, it’s an entirely different matter what YOU feel is best for you. It’s an personal question whose answer depends on your feelings, intuitions, and what you’ve heard and read about different forms of treatment. Additionally, it depends on whether you and the therapist “match” well or not. Remember Sackett’s words about the patient’s own choice and that we must consider the patient’s predicament, rights, and preferences!
With that said, there are certain conditions where the evidence for PDT is most consolidated. A recent “umbrella meta-analysis” (Leichsenring et al., 2023) has focused on the eleven meta-analyses conducted on PDT in the past two years, totaling several thousand patients. They suffered from depression, anxiety disorders, personality disorders, and somatization symptoms. The study was published this year in the leading international journal World Psychiatry. The recommendation according to the EST model (Tolin, D. et al., 2015) for PDT in these conditions was “strong.” Thus, “PDT represents an evidence-based treatment” (Leichsenring et al., 286), with similar evidence to, for example, CBT. We should remember that “no therapy fits all psychiatric patients, as shown by the limited success of all evidence-based therapies” (286). It is usually found that no psychotherapy “cures” more than 50-60% of its patients (e.g., Milrod et al., 2016, Svensson et al., 2021).